The Chain Florey clinician scientist programme
Our Chain Florey programme has been designed to train and develop early career clinician scientists working at the interface of mechanistic discovery research and experimental medicine. The programme supports clinicians to carry out research with LMS discovery science groups while staying in close contact with the clinical environment.

Here at the LMS, we value the important role clinician scientists play in advancing medical research.
The Chain Florey programme was set up in 2009 to offer world-class training to medical graduates, allowing them to develop essential research skills at key stages of their career. The programme has supported many clinicians to combine their medical knowledge with a new-found expertise in scientific research.
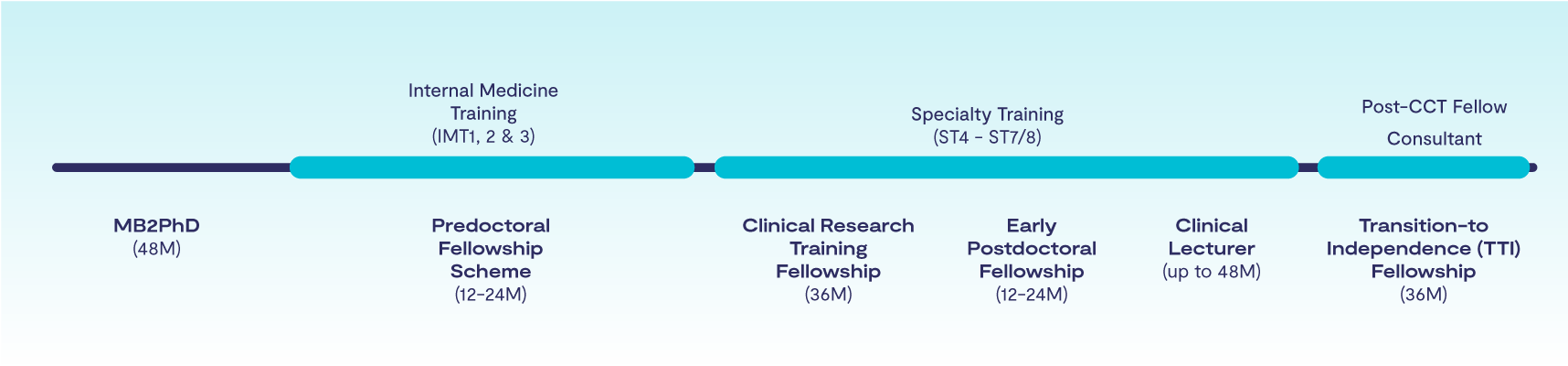
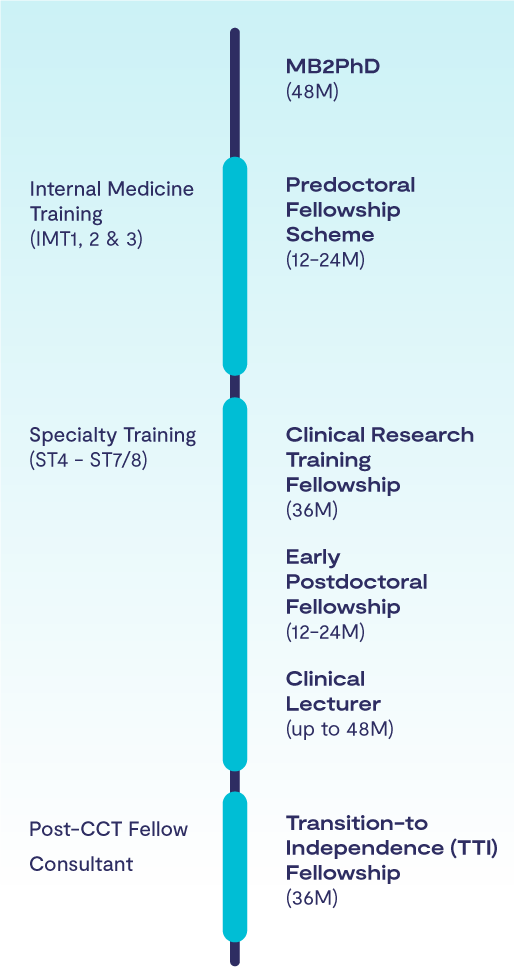
To help navigate the complexities of a clinician scientist career, we have developed a range of Chain Florey fellowships that allow clinicians to experience and undertake research at any point in their career, from graduate to consultant, giving them the support and mentorship they need to flourish.
Chain Florey clinician scientist programme
The Chain Florey programme provides support at various stages of a clinical career, helping individuals develop their research skills and gain research experience, all while continuing their clinical training. We encourage clinicians to explore flexible options, and the programme can offer highly individualised solutions. If you’re interested, do speak to us.
The Chain Florey programme is supported by UKRI and NIHR Imperial Biomedical Research Centre (BRC).
1
Chain Florey MB2PhD
The Chain Florey MB2PhD is for newly qualified doctors who wish to undertake a non-clinical PhD prior to starting Foundation Years training. You will be given the opportunity to spend 100% of your time doing research over four years and will be fully integrated into our LMS PhD Cohort.
2
Chain Florey Predoctoral Fellowship Scheme (IMT 1, 2 and 3 or equivalent)
When you move on to Internal Medicine Training (IMT 1, 2 3; or equivalent for other clinical training pathways), you can apply for our Chain Florey Predoctoral Fellowship scheme. This offers 12 months of full-time research support, or 24 months of research at half-time (50% of your time), allowing you to spend time in the laboratory gaining research training and experience.
3
Chain Florey Clinical Research Training Fellowship (ST4-ST7/8)
A Chain Florey Clinical Research Training Fellowship is usually timed for the phase of your clinical specialty training (ST4-ST7/8), with flexible individual solutions always available. This fellowship offers three years of up to 100% research training, allowing you to fully dedicate your time to laboratory research while working towards a PhD.
We will assist clinicians selected for this scheme in applying for competitive external funding opportunities to help advance their careers.
4
Chain Florey Early Postdoctoral Fellowship (ST4-ST7/8)
To help you transition from completing your PhD to leading independent research, you are eligible for our Chain Florey Early Postdoctoral Fellowship during your specialty training. This fellowship provides between 12 and 24 months of support, allowing you to dedicate 50-100% of your time to advancing your research career. It can also allow you to prepare an Academy of Medical Sciences Starter Grant application, increasing your competitiveness for a clinical lectureship.
5
Chain Florey Clinical Lecturer (ST4-ST7/8)
Upon completing your PhD, you can apply for our prestigious Chain Florey Clinical Lecturer scheme in a specific specialty. This position offers up to four years of research support until completion of clinical training, with 50% of your time reserved for research. Once in post, you can apply for a technician to support your research.
6
Chain Florey Transition-to-Independence Fellowship (Post CCT Fellow, Consultant)
The final step in the Chain Florey pathway is our Transition-to-Independence (TTI) Fellowship, for anyone who has recently obtained or is about to receive their CCT. This unique fellowship supports your transition to becoming an independent researcher leading your own group. It provides three years of support (with consultant level salary), which may include research technician support, allowing you to spend 80% of your time in the lab while continuing to maintain your clinical career as an honorary consultant. This fellowship will help you to develop a highly competitive application for 5-year externally funded intermediate fellowships/research grants.
Who were Chain and Florey?
The legacy of Chain and Florey today
The Chain Florey programme is named in celebration of one of the greatest collaborations between medicine and science: Howard Florey, a clinically trained pathologist, and Ernst Chain, a biochemist, who shared the 1945 Nobel Prize in Physiology or Medicine with Alexander Fleming for their work in discovering, developing and producing the first antibiotic: penicillin.
The Chain Florey Programme has been designed to support the training and career development of early career clinician scientists at the interface of discovery science and experimental medicine. The scheme provides unique opportunities to partner with LMS fundamental discovery science groups and buddy up with early career non-clinical scientists.
Sir Ernst Boris Chain FRS FRSA KBE (1906 –1979)
Chain was a refugee German-born British biochemist. He fled to England in 1933; his mother and sister perished in the Holocaust.
He worked at UCL, Cambridge and then Oxford, where he had a key role in the biosynthesis and purification of penicillin. In 1964, he became the founding Director of the Imperial College Department of Biochemistry where he worked until his retirement.
Howard Walter Florey, Baron Florey OM FRS FRCP (1898 –1968)
Florey was an immigrant scientist; an Australian pharmacologist and pathologist. His team working at Oxford on the production of penicillin for use in humans included biochemists Ernst Chain and Norman Heatley (1911–2004). Florey led the MRC-funded field trials of penicillin during the Second World War, following his successful experimental work in mice and individual patients.
Find out more and apply
At the LMS, we recognise that forging a career in research and balancing this with continuing to develop your clinical career in the NHS can be a challenge. We are committed to inclusivity and recognise that there are many stages in a clinical career where talented and motivated clinicians may lack the support needed to enter research. To address this, we have developed the Chain Florey pathway as a comprehensive support programme, designed to assist clinicians from student to consultant level in making the transition into research. This will help ensure that the best clinicians are given the opportunity to flourish and develop into the world-leading clinician academics of tomorrow. To apply, you will need to submit your CV, publication list, and a project overview that highlights why you're the right person to lead the research and your future plans. Once shortlisted, an interview panel will be organised. Proposed projects should demonstrate potential for collaboration with at least one LMS research group. Feel free to contact the Chair of the Chain Florey Committee, Professor Declan O’Regan (), or the Chain Florey Programme Manager, Aurelie Tromp (), if you would like to find out more or receive advice based on your CV. We welcome anyone with an interest to reach out and discuss opportunities.
Impact of our work
Professor Wiebke Arlt appointed President of the European Society of Endocrinology
Published May 19, 2025
3 Minutes reading time
