The LMS is delighted to announce that Omar El Tokhy, a Chain Florey Fellow, has been awarded an MRC Clinical Research Training Fellowship to further his research into male infertility.
By Emily Armstrong
March 11, 2025
Time to read: 3 minutes
Omar joined the LMS in 2023 to study the genetic basis of human infertility after working at Addenbrooke’s Hospital in Cambridge for four years as a specialty doctor in Obstetrics & Gynaecology, during which time he helped deliver more than 3,000 babies.
Thanks to support from the LMS Clinician Training pathway, the Chain Florey programme, he was able to continue his clinical work as a trainee doctor as he began developing his laboratory research. Omar’s research interests are in understanding the genetic basis for Non-Obstructive Azoospermia (NOA), a genetic condition where men produce no sperm, which affects around 10-20% of men who present with infertility.
Around 15% of couples worldwide experience difficulty in conceiving, with roughly half of cases due to male infertility. The exact causes of NOA are still unknown and there are currently limited treatments available.
“Recent advances in genetic sequencing of infertile patients have identified potential mutations in hundreds of genes that could cause this condition, and this inspired me to delve deeper into verifying these mutations and, with my new fellowship, understanding the mechanisms by which they act to cause infertility,” says Omar.
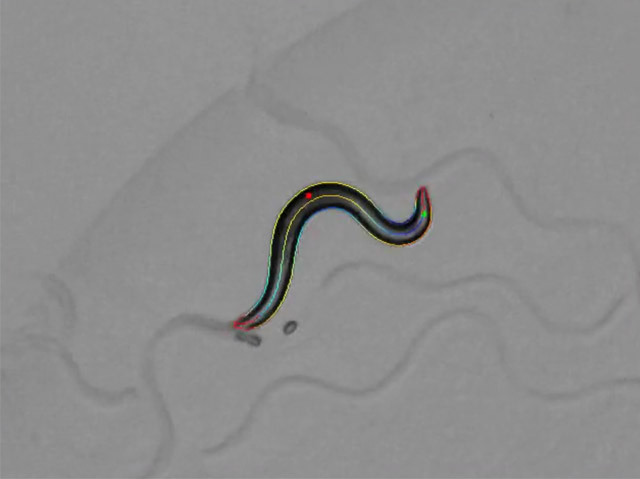
MRC Clinical Research Training Fellowships are highly competitive and provide funding for healthcare professionals across the UK to strengthen their research skills so they can embark on careers as clinical academics. As part of Omar’s new MRC fellowship, he will model mutations that have been identified in people using a microscopic worm called C. elegans.
“Each one of these tiny worms lays around 300 eggs in 3 days, meaning that I can generate a huge amount of fertility data in a short timeframe. The worms are also transparent, which means that I can look at each individual sperm cell under the microscope to help me to understand at which point in its transit things start to go wrong,” says Omar, “What’s more, the way that sperm grow and develop in the worm is remarkably similar to how it happens in men. It really is an amazing model that is tailored to screen lots of human mutations.”
Better understanding how genes contribute to male infertility through research could lead to improved diagnosis and treatment options for couples struggling with infertility. Male infertility is also linked to health problems later in life, such as cancer and other chronic diseases, so in addition to providing future treatments for infertility, understanding NOA could have further reaching implications for men’s health. The condition of having two or more long-term health conditions is known as multimorbidity, and it’s considered one of the greatest challenges to human health in the 21st century. LMS research has a focus on understanding the mechanisms that underlie multimorbidity, with the eventual goal of helping people live healthier and longer lives.
“I am proud, excited and hugely indebted to UKRI and the MRC for allocating funding to allow me to carry out this research, in the hope that we can begin to understand why men are born with no sperm, so that we can offer genetic testing, stratify success of assisted reproductive technology, and perhaps even reverse the genetic disease,” says Omar.