By Sophie Arthur
July 15, 2019
Time to read: 3 minutes
Schizophrenia is a long-term mental health condition that causes a range of psychological symptoms, and is one of the top causes of disability in the world. Schizophrenia affects 1 in 100 people and symptoms can range from memory problems, to auditory and visual hallucinations. But many aspects of the condition don’t have treatments at all, and the treatments we do currently have don’t work very well or patients find hard to take because of the side effects. So, finding a new treatment to treat this condition is of great importance, but to do that we need to understand more fully the causes of schizophrenia itself. The latest research from the Psychiatric Imaging group at the MRC LMS, in collaboration with other European institutes, shares some new insights into how the cannabinoid system contributes to the cognitive impairment of schizophrenia.
Mind and body in balance
The endocannabinoid system (ECS) is one of the brain’s largest neurotransmitter networks. The ECS is always working to achieve balance, or homeostasis, which means maintaining a stable environment regardless of any changes in external stimuli. This whole system is critical to keeping us physiologically healthy, as it can play a role in reproductive systems, sleep, motor control, pain response, memory and mood amongst many more.
The ECS communicates via relays of messengers and receptors. The brain naturally produces endocannabinoid molecules responsible for sending the message to rebalance our bodies, and they look for and activate cannabinoid receptors, just like a lock and key coming together linking your body and brain together. There are primarily two cannabinoid receptors; CB1 and CB2, but it is the CB1 receptor that is much more abundant in the central nervous system.
Previous studies have shown a link between the CB1 receptor and schizophrenia, but in this latest study, researchers wanted to ask whether the availability of the receptor changes at all in patients who is experiencing their first episode with psychotic symptoms without the confounds of cannabis use or illness chronicity.
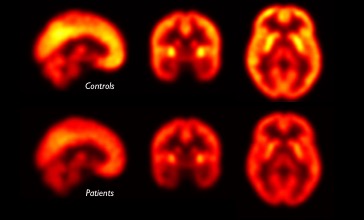
Research published on July 3 in JAMA Psychiatry revealed that the levels of the CB1 receptor were significantly lower in patients with first-episode psychosis. Additionally, the levels of CB1 receptors were linked to symptom severity, with patients with the lowest CB1 receptor levels showing the most severe cognitive impairment.
Prof Oliver Howes, Head of the Psychiatric Imaging group at the MRC LMS and senior author of this study, discussed the next steps for this research:
“This study has shown a link between CB1 receptor availability and the extent of cognitive impairment in schizophrenia patients. This is evidence that the cannabinoid receptor could be a potential new route for treating the disorder. The next steps would be to test whether treatments that targets cannabinoid receptors are effective in helping with cognitive impairment”.
‘In vivo availability of cannabinoid 1 receptor levels in patients with first-episode psychosis’ was published in JAMA Psychiatry on 3 July. Read the article here.
Image taken from JAMA Psychiatry article.