By Sophie Arthur
August 29, 2019
Time to read: 6 minutes
New research shows insights into how our diet and medication impacts our gut bacteria and overall health using a novel screen. Find out more in the article below and in this video:
The gut is home to a vast number of microbes – collectively known as the microbiome. There is accumulating evidence of the crucial role that our gut microbes play in all aspects of our physiology in health and also in disease. The bacteria that lives inside our gut help us to digest food to produce thousands of different metabolites which are crucial for so many vital processes that happen to keep our bodies healthy. But these microbial communities can be directly affected by many lifestyle factors, in particular our diet, and any medication that we may take, which in turn can have a positive or negative impact on our overall health.
We know that nutrition can affect the microbes in our gut which influences our overall health. But we also know that the drugs we take affect our microbiome function and can also affect our health. But there is a piece in the puzzle that is missing. Research published in Cell on 29 August from the Host Microbe Co-Metabolism group at the LMS reported how nutrients, drugs and the microbiome interact together and influence host health.
Dissecting the complexity with a new screening tool
Trying to effectively understand the effects that each of these factors has on host health is very complex due to the possible direct and indirect effects they can each have, but also because of all the vast numbers of nutrients that exists in the food we eat. Researchers at the LMS developed a new high-throughput screening tool to unpick and define all these thousands of interactions – an automated procedure that allows you to test all possible combinations much more quickly.
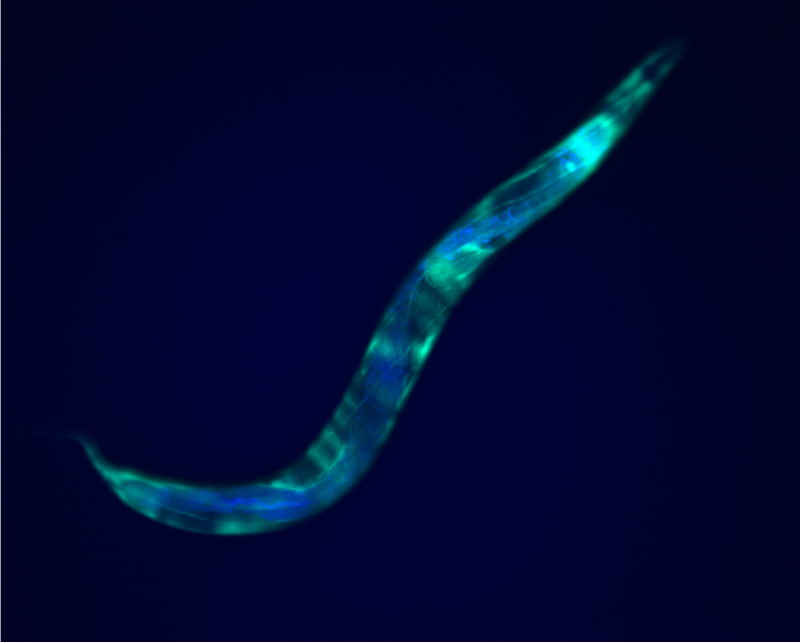
This study reports this new tool that incorporates the four key elements needed to dissect this question. First, the drug metformin was chosen as it is known to impact the microbiome, and it is used to treat diabetes and also ageing. Additionally, a study has previously shown that diabetic patients using metformin had decreased mortality compared to healthy patients1. Second, food was broken down into its individual nutrient elements and added in succession throughout the screen. Third, the bacteria E. coli was used to represent the microbiome as it is present in the gut of most healthy humans. Finally, C. elegans was used as the host organism as many of the processes that exist in humans, are also present in this nematode worm.
From worms, to flies, to humans
Researchers found that, like human cells, E. coli was able to integrate signals from drugs and nutrition to influence overall host health by forcing alterations to which metabolites the microbiome produced. Analysis of the metabolites revealed which classes of nutrients brought the desired metabolic response in the host. Sugars were found to shut down the activation of a transcription factor, a protein that binds to the DNA at a specific site to turn on relevant genes, which would lead to downstream adaptation of metabolism. On the other hand, amino acids and other nitrogen-containing nutrients helped activate these downstream effects induced by the drug.
To determine whether this signalling pathway could be exploited in humans as a possible target for the treatment of metabolic diseases, the team wanted to understand if this mechanism observed in worms was an evolutionarily conserved trait.
First, in collaboration with the Redox Metabolism group here at the LMS, the key findings were investigated in the model organism Drosophila melanogaster, also known as the fruit fly, acting as the host. Researchers observed that flies colonised with E. coli and treated with metformin had a longer lifespan. Thus, the microbiome was regulating the host health by once again integrating the signals from nutrition and the drug.
Further to this, in collaboration with Christoph Kaleta’s group in Germany, dietary information, metformin administration status and information about the gut microbes was collected from healthy patients and those with type-2 diabetes. Using all these parameters together, researchers devised a computational approach to determine whether the presence of a particular microbe in the human gut meant that a patient was more or less likely to produce a particular metabolite when taking metformin.
Christoph Kaleta, senior author on this study, discussed the human modelling approach:
“We were intrigued by the results in the worms and wondered whether they also apply to the much more complex microbiota of humans. From the samples we collected, we determined which bacteria could be found in the gut of each participant and translated them into computer simulations of the gut microbiome. From this modelling approach, we found that patients taking metformin and who had E. coli present in their gut microbiome were able to produce more of those nitrogen-containing compounds that can help improve overall host health.”
Paving the way for new treatments
The findings provide one possible explanation as to why diabetic patients taking metformin have increased survival compared to healthy patients and could optimise drug function by adapting the diet of the host forcing them to produce key metabolites. It also paves the way to develop new drugs that can target bacterial signalling pathways that will again force the production of key nutrients to improve host health.
Filipe Cabreiro, Head of the Host Microbe Co-Metabolism group at the MRC LMS, discussed the next steps for this research:
“Our new screening technology has helped uncover the metformin specific metabolic and bacterial signalling pathways that regulate host metabolism. However, what is still unknown, is the biological target that metformin inhibits leading to this cascade of events and that is what I am keen to investigate next”.
‘Host-Microbe-Drug-Nutrient screen identifies bacterial effectors of metformin therapy’ was published in Cell on 29 August.