By Helen Figueira
September 22, 2010
Time to read: 4 minutes
 Gene Regulation and Chromatin
Gene Regulation and Chromatin
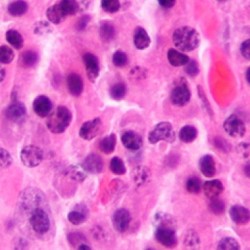
Plasma cells are white blood cells that carry huge payloads of antibodies, affording us long-lasting protection against infections. The regulation of plasma cell lifespan is critical for maintaining a controlled immune response. Researchers in the Gene Regulation and Chromatin group have recently identified a novel mechanism that is involved in determining the timing of plasma cell death.
The immune response produces two types of plasma cells. In response to antigens, short-lived plasma cells are formed rapidly in secondary lymphoid organs such as the spleen and die after only a few days of intense immunoglobulin secretion. In contrast, long-lived plasma cells survive in the bone marrow for much of the lifetime of an organism to provide long-term immunity. Production of antibodies by both types of plasma cells is thought to contribute to the development of autoimmune diseases. While the longevity of bone marrow plasma cells is partly due to survival signals provided by the bone marrow microenvironment, the mechanisms that determine the lifespan of short-lived plasma cells have so far remained elusive.
When B cells differentiate into plasma cells, they expand their endoplasmic reticulum (ER) and Golgi dramatically to accommodate high-level antibody production and secretion. The study, carried out by Holger Auner and Pierangela Sabbattini and published in Blood, shows that despite this expansion, short-lived plasma cells suffer from substantial and progressively increasing stress on the endoplasmic reticulum (ER stress). This ER stress, which can occur in any cell type, results from the accumulation of faulty (misfolded) proteins. In plasma cells, ER stress is caused by high-level antibody secretion and ultimately triggers cell death if the toxic peptide “garbage” cannot be cleared up. In most cell-types, this is achieved by slowing down protein production for a period. However, this is not an option for plasma cells, which need to maximise antibody output. So, how do plasma cells deal with ER stress, which is brought about by their own function of producing antibodies?
The team found that short-lived plasma cells, instead of activating the protective mechanisms that prevent ER stress, keep themselves alive by blocking the activation of the effector caspases that normally trigger programmed cell death (apoptosis). Active effector caspases cleave hundreds of cellular proteins during apoptosis in order to dismantle the dying cell in an orderly fashion. The conventional view has been that there is no apoptosis without activation of effector caspases. However, Auner et al. found that caspase-9 and caspase-3 are not activated in plasma cells in response to death stimuli, including ER stress. They also observed that a tri-aspartic acid repeat within caspase-3, which blocks inappropriate activation of caspase-3 in healthy cells, is stabilised in plasma cells. The cells do ultimately succumb to the effects of ER stress but this occurs without activation of the effector caspases.
The results of this study provide evidence for a novel mechanism for regulating the timing of programmed cell death in plasma cells. When high-level antibody secretion causes a progressive increase in ER stress, apoptosis is blocked by the failure to activate the key effector caspases. This allows plasma cells to remain functional and maintain antibody output. Ultimately, ER stress becomes overwhelming and mediates plasma cell death through alternative mechanisms. The combined effects of ER stress and the block on caspase activation appear to fine-tune the timing of plasma cell death. The CSC researchers also found evidence that caspases can be resistant to activation in multiple myeloma (an incurable plasma cell malignancy), a finding that could be important for understanding responses of these cells to chemotherapy.
These findings pave the way for further investigations into how the interplay between ER stress and the block on caspase activation affects the survival of short-lived plasma cells and how this impacts on conditions such as autoimmune diseases and multiple myeloma.
Auner, H.W., Beham-Schmid, C., Dillon, N. and Sabbattini, P. (2010). The life-span of short-lived plasma cells is partly determined by a block on activation of apoptotic caspases acting in combination with endoplasmic reticulum stress. Blood, in press. link to article