By Helen Figueira
April 27, 2015
Time to read: 4 minutes
Deborah Oakley
Scientists have identified an enzyme that plays a critical role in the way our bodies react to sepsis, a condition in which the immune system can go into fatal overdrive after infection.
Understanding more about the way this enzyme works could lead to cheaper, more effective drugs – and save lives. It could also help doctors to deal with antibiotic resistance and auto-immune conditions such as rheumatoid arthritis and atherosclerosis.
Sepsis is one of our biggest killers. Government figures suggest some 80 people a day die from sepsis in England alone, more than the top three cancers put together, and that better diagnosis and treatment could save around half of these.
But doctors warn that for the situation to improve, scientists will need to develop a far deeper understanding of the condition itself. Now, for the first time, researchers at the MRC’s Clinical Sciences Centre (CSC) in West London have homed-in on an important mechanism behind the process.
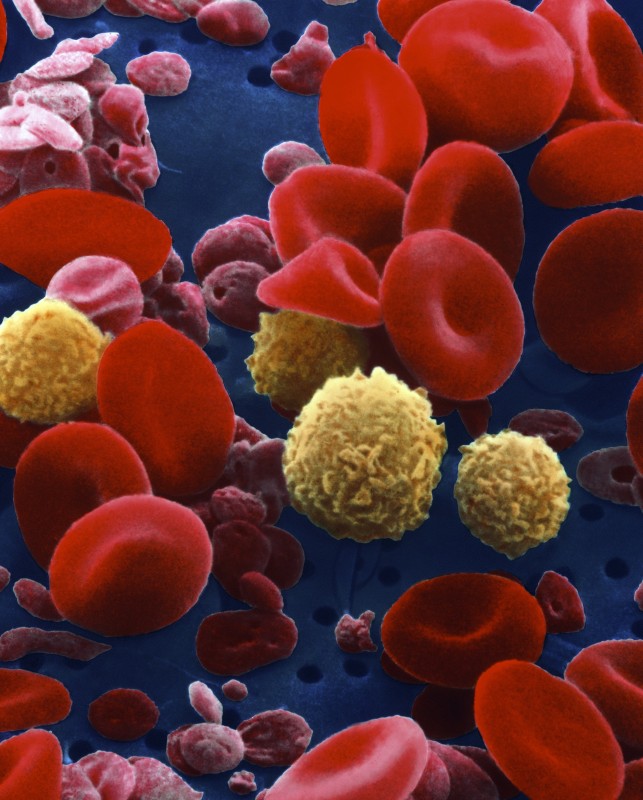
Sepsis occurs when harmful bacteria infect a patient’s blood stream and release toxins. The body’s immune cells attack the bacteria to control the infection. They are activated by a chemical called nitric oxide. But this same chemical is vital in keeping our blood vessels flexible.
The amount of nitric oxide our bodies produce is critical. Too little and our immune cells will struggle to tackle bacteria. Too much and our blood vessels can become leaky, may collapse, and eventually cause the multiple organ failure associated with sepsis. It’s a delicate balance.
The team at CSC has identified the cellular controller behind both processes – an enzyme called DDAH2.
“What’s exciting about this research is that we’ve shone a light on a new way that our bodies respond to bacterial infections,” says James Leiper of the CSC’s Nitric Oxide Signalling group, who led the research. “This gives us confidence that we will be able to design new drugs to treat sepsis.”
Growing concern about the rise of antibiotic resistant bacteria makes the work, published this month in Arteriosclerosis, Thrombosis and Vascular Biology, particularly timely. “At the moment, we rely on antibiotics to treat people with sepsis. But as we face the challenge of antibiotic resistant bacteria it is vital that we find new approaches, and new drugs, to help such patients,” Leiper explains.
The team used mice engineered so that they did not produce the crucial DDAH2 enzyme, to test their suspicions that the enzyme is key. Without the enzyme, mice were much more susceptible to sepsis. To find out which cells are critical, the scientists next removed DDAH2 from the immune cells. Again, the mice were unable to fight off sepsis, confirming that immune cells play a key role in determining the outcome of sepsis.
The animal models were especially relevant because they allowed the researchers to mimic the way that sepsis develops in real-world situations, for example following gastric surgery when a patient’s bowel might leak – a common cause of sepsis.
Leiper and his team plan to explore the possibility of developing drugs tailored to work in people whose genes make them unusually susceptible to sepsis. Last week, doctors writing in The Lancet Infectious Diseases warned that sepsis is one of the best known yet most poorly understood medical disorders. One of their recommendations is the use of such genetic approaches to develop targeted, ”personalised medicine”.
There could be even wider application for the CSC team’s work – in chronic inflammatory conditions, such as rheumatoid arthritis and atherosclerosis. In such conditions, having highly activated immune cells is not good news because they attack the body’s own tissue.
Dampening down this process is key, but current drugs are expensive and effective only in some patients. If scientists can inhibit DDAH2, they may be able to reduce levels of nitric oxide produced in immune cells, and so stop these cells from being activated. This may prove to be a cheaper way to target all patients.
“We have preliminary evidence in animal models that inhibition of nitric oxide can improve outcomes of rheumatoid arthritis,” says Leiper. “This approach may prove more effective than current drugs, which are expensive and only work for a subset of patients.”
Funding for the research came from MRC Technology, the commercial arm of the MRC.
For further information, please get in touch:
Susan Watts
Head of Public Engagement and Communications
MRC Clinical Sciences Centre
Du Cane Road
London W12 0NN
T: 0208 383 8247
M: 07982 142327
E:
Deborah Oakley
Science Communications Officer
MRC Clinical Sciences Centre
Du Cane Road
London W12 0NN
T: 0208 383 3774
E: