By Helen Figueira
October 31, 2016
Time to read: 5 minutes
By Deborah Oakley
Scientists have shown that a mutation in a gene called Arid1b can cause liver cancer. Arid1b normally protects against cancer by limiting cell growth, but when mutated it allows cells to grow uncontrollably. The researchers have shown that two existing drugs can halt this growth in human cells. This points to a new approach to treating liver cancer.
These early results could be translated into a treatment relatively quickly, says Jesús Gil of the MRC Clinical Sciences Centre (CSC), based at Imperial College London, and who led the study. This is because the drugs are already used to treat other types of cancer. Gemcitabine is used on bladder, pancreas and ovary cancer, whilst DON has been tested in clinical trials. Both are known to be safe in people so will not require the usual toxicity testing.
According to MacMillan Cancer Support, 4,200 people in the UK are diagnosed with liver cancer annually. “Liver cancer is a deadly disease,” says Luca Tordella, a postdoctoral researcher at the CSC who played a key role in the study. He says the new treatment will be most effective in people who have a mutation in the Arid1b gene. “It’s important to better classify patients into groups, according to their genes. One advance of personalised medicine is to understand which drug will work best on you, and which on me.”
The CSC team began by looking for mutations in the DNA of 100 people with liver cancer. They focused in on genes known to regulate a cellular state called senescence. This is a built-in safety mechanism that helps to protect the cell against cancer. Senescence is triggered when a cell grows abnormally fast and, once induced, it acts to keep the cell in limbo, such that it is alive but can no longer grow or divide. Bypassing senescence is a hallmark of many types of cancer.
The researchers initially identified 300 mutations, each of which effectively turned off a gene. But not all mutations are harmful. To find out which of these mutations might disrupt senescence, they worked with researchers at the University of Tübingen, Germany. Together they turned off each gene, one at a time, in a type of mouse cell called a fibroblast. These cells are widely used for studying senescence.
When they turned off the Arid1b gene, the mouse cells could no longer enter senescence. It has previously been suggested that a mutation in Arid1b plays a role in liver cancer and now the CSC team shows that it does so by disrupting senescence.
To confirm its role, they mutated it in mice that also had a mutation in the gene Ras, which is known to cause various types of cancer. Together, the Ras and Aridb1 mutations made the mouse’s cells grow faster than normal and bypass senescence. Eventually, the mice developed liver cancer.
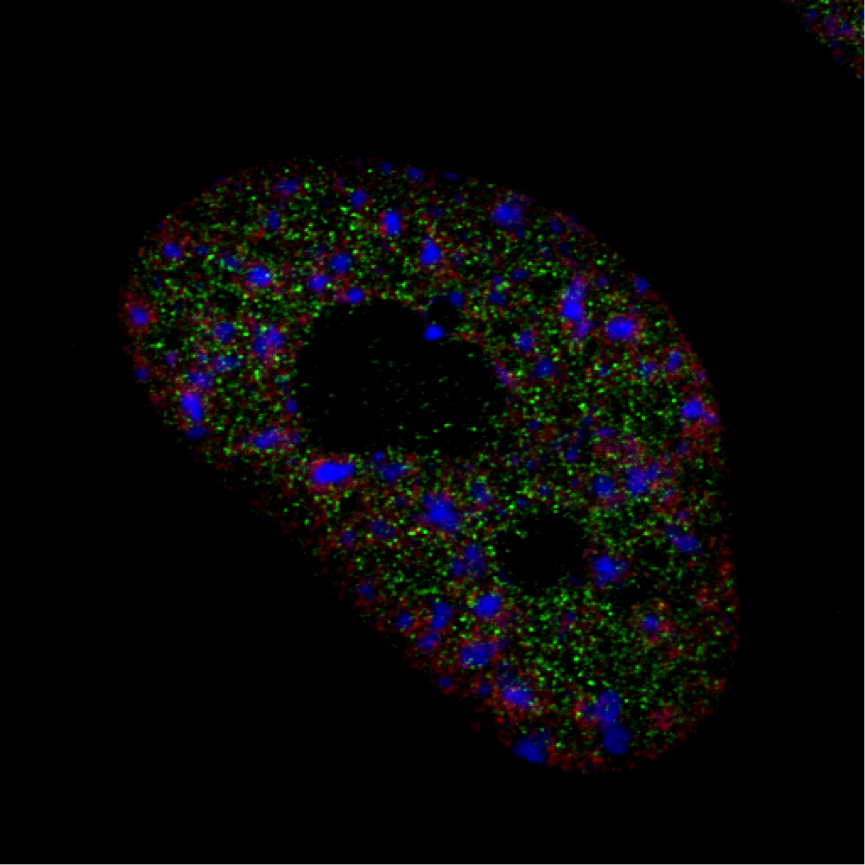
Then, to check that the Arid1b mutation has the same effect in people, the researchers mutated Ras and Arid1b in human fibroblast cells. As expected, the cells grew rapidly and didn’t enter senescence.
According to Tordella, it’s been suggested that the Arid1b gene produces a protein which joins with others to form a group, called the SWI/SNF complex. This complex triggers senescence, but it has not been known how exactly this happens.
Now the CSC team has shown that the SWI/SNF complex regulates the activity of hundreds of genes, including three that control senescence. One of these genes, Entdp7, produces an enzyme that breaks down the building blocks that a cell uses to build DNA strands. Without these blocks, called nucleotides, the cell cannot copy its DNA, and so cannot grow and divide. It enters senescence.
But if Arid1b is mutated, as it is in some liver cancers, the SWI/SNF complex will not form and the Entdp7 gene will not be activated. This means there will be no enzyme to degrade the nucleotides, and the cell can continue to build more DNA strands, allowing it to grow and replicate. In this way, Gil and Tordella have found a mechanism by which mutations in Arid1b can lead to cancer.
They have also shown that this can be treated. When they gave cells with an Arid1b mutation either the drug gemcitabine or DON, the cells began to break down nucleotides, thereby triggering senescence. This stopped cancer in its tracks.
“Around 20% of patients with liver cancer have mutations in the SWI/SNIF complex. What we suggest is if we treat these people with drugs that target the degradation of nucleotides, they will respond,” says Gil. “We plan to continue to research this in the lab to develop treatments to target liver cancer.”
Read the full paper here.
To find out more get in touch:
Deborah Oakley
Science Communications Officer
MRC Clinical Sciences Centre
T: 0208 383 3791
M: 07711 016942
E: