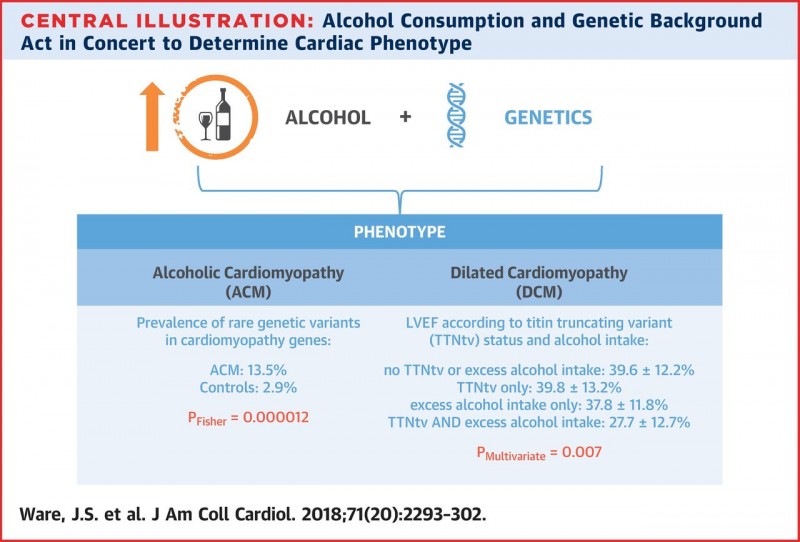
Alcohol Consumption and Genetic Background Act in Concert to Determine Cardiac Phenotype: Alcoholic cardiomyopathy (ACM) patients exhibit a higher prevalence of rare variants in dilated cardiomyopathy (DCM)-associated genes than control subjects. In DCM patients, neither the presence of a titin truncating variant (TTNtv) nor excess alcohol consumption had a significant effect on baseline left ventricular ejection fraction (LVEF) in isolation, but the combination was associated with a significantly lower baseline LVEF. Values shown are absolute ejection fraction in each group. The p value is derived from multivariate analysis.
Researchers have found an important underlying genetic component of alcoholic cardiomyopathy (ACM), a condition previously believed to be due solely to the toxic effects of excessive drinking.
Alcoholic Cardiomyopathy (ACM) is a common cause of dilated cardiomyopathy (DCM) characterised by the left ventricle of the heart becoming dilated (stretched or ‘baggy’). As a result, the heart muscle becomes weak, thin or floppy and is unable to pump blood around the body efficiently.1
Research published in the Journal of the American College of Cardiology by Ware et al., builds upon the pioneering work of the authors on the genetics of heart failure and the influence of environmental factors on genetic predisposition.
Excess alcohol consumption has been implicated in up to 40% of cases of DCM.2 However, the factors which determine cardiac toxicity on exposure to alcohol and the genetic component of ACM were largely unknown.
Dilated cardiomyopathy is estimated to affect up to 1 in 250 individuals, is a major cause of heart failure and the leading cause of transplantation in the UK.
The study was conducted by MRC LMS researchers James Ware, Declan O’Regan and Stuart Cook in collaboration with colleagues in London and Madrid. Including groups from National Heart and Lung Institute, Imperial College London and Royal Brompton and Harefield NHS Foundation Trust London.
To explore the genetic component of ACM the researchers investigated the genetic variation in known DCM-causing genes. To do this they compared the genetic variation of the DCM-causing genes of 141 individuals with ACM, with 366 individuals with DCM, 445 healthy volunteers and population-based frequency data.
They identified that the prevalence of genetic variants for DCM-causing genes was significantly higher for ACM individuals (13.5%) compared to healthy volunteers (2.9%). The rate of genetic variation for healthy volunteers was as expected for the general population.
The gene encoding titin (titin truncating variants (TTNtv)) known to be the predominant genetic cause of dilated cardiomyopathy, accounted for the majority of variants detected in ACM cases and was found at a similar frequency seen in DCM cases.
The authors found that genetic predisposition alongside excess alcohol consumption is associated with increased severity of disease in DCM patients. These findings support that alcohol and other environmental factors interact with genotype to determine cardiac phenotype.
The researchers conclude that clinical screening and genetic testing should be considered for patients and family of patients presenting with ACM. A topic which was the subject of the editorial of the journal written by Mariann R. Piano, Nancy and Hilliard Travis Professor of Nursing, Vanderbilt University.
You can read the article in full here: http://www.onlinejacc.org/content/71/20/2293
References
1 https://www.bhf.org.uk/heart-health/conditions/cardiomyopathy/dilated-cardiomyopathy
2 Guzzo-Merello et al., Natural History and Prognostic Factors in Alcoholic Cardiomyopathy, JACC: Heart Failure, Volume 3, Issue 1, 2015, Pages 78-86, ISSN 2213-1779, https://doi.org/10.1016/j.jchf.2014.07.014.
Article: Ware et al., Genetic Etiology for Alcohol-Induced Cardiac Toxicity Journal of the American College of Cardiology May 2018, 71 (20) 2293-2302; DOI:10.1016/j.jacc.2018.03.462
