Researchers from Cambridge University and the MRC Laboratory of Medical Sciences find that healthy blood vessels contain a small number of “primed” smooth muscle cells that are predisposed to respond to vascular inflammation and injury. Targeting these primed cells can be a promising therapeutic approach for preventing and treating vascular diseases such as atherosclerosis.
 Vascular smooth muscle cells (VSMCs) are normally resident within the vascular wall and are involved in the contraction of the blood vessels. However, in response to inflammation or injury these cells adopt a special “synthetic” phenotype characterised by active proliferation and migration in order to repair the injury site. This process of so-called “VSMC phenotypic switching” is dysregulated in atherosclerosis, where VSMCs divide actively, giving rise to large numbers of “synthetic” cells that form the bulk of atherosclerotic plaques.
Vascular smooth muscle cells (VSMCs) are normally resident within the vascular wall and are involved in the contraction of the blood vessels. However, in response to inflammation or injury these cells adopt a special “synthetic” phenotype characterised by active proliferation and migration in order to repair the injury site. This process of so-called “VSMC phenotypic switching” is dysregulated in atherosclerosis, where VSMCs divide actively, giving rise to large numbers of “synthetic” cells that form the bulk of atherosclerotic plaques.
“Atherosclerosis may have no symptoms at first, but can eventually lead to heart attacks and strokes, which is why studying VSMC phenotypic switching is very important,” says Dr Mikhail Spivakov, the Functional Gene Control Group Leader at the MRC LMS and a co-author of the study.
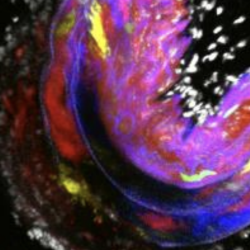
The Cambridge team (led by Dr Helle Jørgensen) had previously found that VSMCs within the atherosclerotic plaques are the clonal offspring of only a small number of cells. The new study investigates this phenomenon by looking at what happens when VSMCs are exposed to vascular injury. Using a combination of single-cell transcriptomics and imaging, the authors observe that while many VSMCs acquire “synthetic” features to different degrees after injury, only a small number of them start dividing. Notably, the authors found that an intermediate state on the cells’ progression to the actively dividing state corresponds to the rare cell population of Sca1-expressing VSMCs that they had previously identified in healthy blood vessels. When tested experimentally, these cells grew more readily, consistent with the hypothesis that Sca1-expressing VSMCs may be present in a primed state that predisposes them to respond to inflammation.
The above analysis has been performed in mouse and, notably, the human genome does not have the equivalent of the mouse Sca1 gene that made it possible to distinguish the primed VSMCs. Therefore, the authors defined a broader expression signature of these cells that contained genes also found in humans and used it to confirm the presence of an equivalent population in humans.
Synthesising these findings, the authors propose that vascular cells that are present in the primed state at the point of injury would be more likely to respond through active proliferation and changes in their gene expression and behaviour. This would explain why only a small number of VSMCs actively participate in the injury response.
“Importantly, we don’t think that the primed cells represent an entirely separate subtype of VSMCs,” stresses Spivakov. “Rather, we believe that VSMCs in healthy blood vessels could become primed by chance, due to some yet unknown intrinsic fluctuations or external cues”.
“From the clinical perspective, our results suggest that inhibiting the intermediate state of VSMCs therapeutically may be a potential new way for preventing or treating atherosclerosis that is characterised by overactive VSMCs, as well as for minimising the adverse effects of recurring stenosis post-surgery,” says Dr Helle Jørgensen, a group leader at Cambridge University’s Department of Medicine and the study’s corresponding author.
This research was funded by a British Heart Foundation grant to the Jørgensen and Spivakov labs and was published in Cardiovascular Research on 22 August 2022.
